1. Predictable:
- Excessive Pharmacological Effects.
- Secondary Pharmacological Effects.
- Rebound Response on Discontinuation.
2. Unpredictable:
- Allergic reactions and anaphylaxis.
- Idiosyncrasy.
- Genetically determined effects.
Excessive Pharmacological Effects
It is the most common adverse drug reaction which may
occur due to the excessive pharmacological effect of the drug. The excessive
pharmacological effect generally appears due to the overdosage of a drug. This
is particularly troublesome with cardioactive, hypotensive, hypoglycemia, and central nervous system
depressive agents. For example, a hypotensive agent used in hypertension, in
excess dose cause profound hypotension. Adverse reactions due to excess
pharmacological effects may also appear at the usual therapeutic dose in a certain
condition. These include:
• Patients with kidney disease particularly those who have
lost more than 70% of kidney function.
• Hypoalbuminemia which may be due to failure of
albumin production as in liver disease or albumin loss as in nephrotic
syndrome.
• Patients at the extremes of the age range, i.e.
infants and neonates. Adverse reactions
in these conditions can be minimized by dose adjustment after knowing the
pharmacokinetic behavior of an administered dose.
Secondary Pharmacological Effects
No drugs have a single pharmacological effect. Any
effects which are associated with a drug
besides the desired effects are called secondary effects. Drugs have several
pharmacological actions at the usual therapeutic dose but it is prescribed
solely for one of these beneficial actions. For example;
• Antihistamines are prescribed for their
anti-allergic skin reactions or their antinausea effects, but they also produce
drowsiness due to central nervous system depression (secondary pharmacological
effects). This action may be of little importance for patients lying in bed but
it may have disastrous consequences if a
patient is the motor driver. This effect may be greatly exacerbated if
the patients are also taking hypnotics, tranquilizer, and cough suppressant as
medicines or is consuming alcohol.
• Loss of potassium or extra-cellular fluid
concentration following thiazide diuretics therapy in treating
hypertension.
• Therapeutic dose of salicylates is as potent as some
of the sulfonylureas in lowering blood glucose levels in both diabetic and
non-diabetic patients.
Idiosyncrasy
The term idiosyncrasy (Greek idios, which means “one’s
own; and synkrasis, a mixing together”)
has long been used to denote both quantitative and qualitative abnormal
drug response. Idiosyncrasy covers
unusual, bizarre, or unexpected drug effects which cannot be explained or
predicted in individual recipients. It also includes drug-induced fetal
abnormalities e.g. phocomelia, which developed in the offspring of others
exposed to thalidomide. Drug-induced cancer is also an idiosyncratic reaction.
Other examples of idiosyncrasy include:
• Analgesic may induce tumors of the kidney pelvis in
patients with renal disease. Long-term therapy with immunosuppressive agents
like azathioprine, and cyclophosphamide may induce lymphoid tumors.
• Thyroid cancer may develop in Patients who have
received 131I therapy in the past.
Characteristics of idiosyncrasy, allergy, and toxicity
are compared in the table given
below:

Table.1: Comparisons between Idiosyncrasy, Allergy, and Toxicity
Allergic Drug Reactions
Allergy is an adverse response to a foreign substance
resulting from previous exposure to that substance. It is manifested only after
a second or subsequent exposure. Only a small proportion of the population
exposed to the drug exhibit allergic reactions. Characteristics of allergic adverse drug reactions are as
follows:
• The reaction does not resemble the expected
pharmacological action of the drug.
• There is a delay between the first exposure to the
drug and the development of a
reaction.
• The reaction recurs on repeated exposure even to minute
quantities of the drug.
The mechanism of allergic drug reactions can be
explained on an immunological basis. Drug or its metabolite which is a small
molecule having a simple structure generally combines with body proteins. This
stable drug-protein complex act as an antigen. Simple chemicals which are
capable of binding firmly with a protein to form antigen products, are termed ‘haptens’.
When an individual comes in contact with an antigenic
complex, there occurs the formation of antibodies; i.e. sensitized. Such
sensitized individual when re-exposed to the drug or hapten, antigen reacts with antibodies.
Antigen-antibody complex triggers the release of mediators like histamine from
mast cells. Now manifestations of allergic reactions occur which are
characteristics of the mediator and not the drug. Common allergic drug
reactions in humans are summarized in the table below:
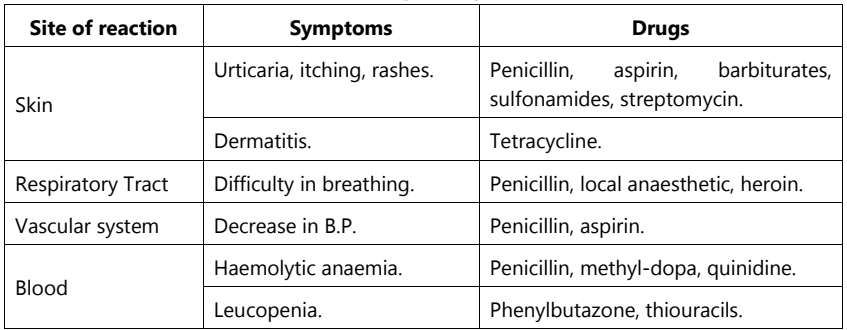 |
Table.2: Common Allergic Drug Reactions in Human |
‘Anaphylaxis’ is the most serious type of drug allergic reaction. It occurs only after second or subsequent exposure to the drug causing the allergy. It is generally due to Immunoglobulin E (Ig). Anaphylactic reactions are shown by Penicillin, anesthetics, dextran, and iodine-containing compounds. The allergic response may be generalized or localized. Generalized anaphylaxis is characterized by bronchospasm, circulatory collapse with hypotension, and sometimes a skin rash. If it is localized to the gut, shows abdominal pain in the bronchi, shows asthma.
In the most severe form of anaphylaxis, ‘anaphylactic
shock’ death may occur within a few minutes due to complete obstruction of
respiratory passages and lowering of blood pressure. Anaphylaxis may be severe after intravenous
administration of the drug; this may be of the massive antigen-antibody
reaction. When the drug is given by other routes, its access to antibody
molecules is necessarily slower.
Genetically Determined Toxicity
Patients of selected genetic makeup are at
substantially greater than average risk for some specific drug toxicities. For
example, glucose-6-phosphate dehydrogenase is involved in the degradation of
glucose for producing energy. Certain populations in Africa and South East Asia are deficient in glucose-6-phosphate
dehydrogenase and, therefore, there is a substantial risk of developing hemolytic
disease after the use of antimalarial drugs – primaquine, sulphonamides, guanidine, and nitrofurantoin.
Similarly, there is other genetically determined toxicity. These include:
• Patients with porphyria are susceptible to CNS
depression agents like barbiturates.
• Individual with pseudocholinesterase deficiency is
highly susceptible to succinylcholine. They may develop paralysis and often
apnoea.
• Many drugs are detoxified in the liver by
acetylation. The ability of acetylation of many drugs in the liver is variable
between individuals. Slow acetylators have a greater risk of toxicity for some
drugs like; isoniazid, procainamide, hydralazine, phenelzine, and dapsone.
Toxicity Following Sudden Withdrawal of Drugs
Tolerance occurs after prolonged use of a variety of
drugs including narcotic analgesics, hypnotics,
ethyl alcohol, some hypotensive agents (clonidine), and corticosteroid
drugs. Sudden withdrawal of such drugs shows severe adverse effects.
In patients habituated to central nervous depressants
such as; ethyl alcohol, barbiturates, and some benzodiazepines, withdrawal of
the usual dose may produce marked agitation,
tachycardia, confusion, delirium, and convulsions. Clonidine is used in
hypertension but its sudden withdrawal may cause severe hypertension.
Long-term corticosteroid therapy is less common
because it may cause atrophy of the recipient’s adrenal glands. Therefore,
sudden withdrawal can precipitate an acute adrenal crisis (Addison’s disease)
in which the patients become profoundly weak, have hypotension, and are
collapsed. Such circumstances can be avoided by gradual removal of the
corticosteroid over weeks depending upon the length of time they have been
consumed.
Drug Interaction
Drug interaction may be defined as an alteration of
the effects of one drug by prior or concurrent administration of another drug.
Apart from the interaction of a drug with another drug (drug-drug interaction), with food (drug-food
interaction) and disease state (drug-disease interaction) it also
includes.
Drug interaction becomes clinically more significant
in patients with renal impairment,
alcoholics, and patients receiving chronic medication or having
metabolic abnormalities. Drug
interaction may become harmful to the patient by increasing efficacy or
toxicity or by decreasing the therapeutic effect of an administered drug. But
sometimes interactions may prove beneficial; when it allows a reduction in dose
by enhanced efficacy without increased toxicity.
Certain drug groups like; anticoagulants, oral
hypoglycemic agents, cytotoxic drugs,
digitalis, and monoamine oxidase inhibitors show a large number of drug
interactions. Drug interactions are
classified in the following ways:
Consequences Wise
They are classified into two categories:
• Beneficial
• Adverse drug interaction
Some drug interactions may be desirable and intended when
a combination of medications produces improved therapy, perhaps a greater
margin of safety, more appropriate onset or duration of action, lowered
toxicity, or enhanced potency with diminished side effects. Such an interaction
is also termed an Intentional Drug Interaction. Beneficial interactions are not frequently reported but
in certain conditions, they have been used to minimize the risk of a particular
form of therapy or to improve its therapeutic efficacy, for example:
• Combination of sulphamethoxazole with trimethoprim
is used to enhance the antibacterial effect of either therapeutic effect.
• Combination of different hypotensive drugs (e.g.
β-receptor blocking drugs and diuretics) is used to get additive effects.
• Combination of different antibiotics (e.g.
ampicillin and cloxacillin) is in practice for better results.
• Various types of cytotoxic drugs are used in cancer
therapy to increase therapeutic efficacy.
Adverse Drug Interaction results in drugs that
antagonize each other. Example of this type of interaction includes morphine
and nalorphine (opposite physiological action),
cholinesterase inhibitors, and atropine (opposite physiological action).
Site Wise
Based on the site, the adverse reactions may be
external or internal.
External: There
are many physical and chemical incompatibilities when drugs are mixed in
infusions, vials, syringes, etc.
Precipitation or inactivation may occur.
Internal:
In this adverse reaction is at the body site or system (e.g. gastrointestinal
tract, liver) or site of drug action (e.g. cell membrane, receptor site). For
example, atropine competitively blocks action at muscarinic receptors, and co-administration
of penicillin and tetracycline (HCl)
causes precipitation in the intravenous fluid. Penicillin causes the
inactivation of gentamicin if given together in the intravenous fluid.
Mechanism Wise
Drug interactions can be classified based on their
mechanism i.e. pharmacokinetic drug interaction and pharmacodynamic drug
interaction.
Pharmacokinetic Drug Interaction: It
occurs as a result of altered drug absorption, distribution, metabolism, and
excretion.
Altered Drug Absorption:
It may be due to the following reasons:
• Physiochemical Interaction: Change in gastric
pH by one drug (e.g. antacid cimetidine, ranitidine) which affects the
ionization of another drug and so absorption of aspirin remains unionized at
the stomach pH, so the drug is rapidly absorbed from the stomach but the use of
antacid with aspirin reduces the absorption due to alteration of pH.
Chelation of tetracycline in patients receiving
iron/calcium preparation occurs, which results in poor absorption.
Activated charcoal absorbs many drugs in the stomach
and so prevents their absorption.
• Altered Gastrointestinal Motility: It affects
the rates of drug absorption. For
example, propantheline which delays gastric emptying and reduces intestinal motility
will cause hindrance in the absorption of many drugs, e.g. digoxin, and quinidine. Similarly, narcotic analgesics, e.g. morphine
may delay the absorption. Metoclopramide
increases gastric emptying and intestinal motility and so causes rapid
absorption of the drug from the upper small intestine.
• Change in Bacterial Flora: Intestinal flora
may play important role in synthesizing vitamin K, essential for normal blood
clotting, or may reactivate some inactive drug metals excreted via bile by
deconjugating them. Antibiotics may interact with these drugs by modifying or
eliminating intestinal flora.
• Change in Mucosal Function: Drugs with
specific gastrointestinal tract toxicity
(e.g. colchicine) may damage the gastrointestinal mucosa or block active
transport and so alter the absorption rate of the drug.
• Blood Flow: The better the blood supply to an
area where a drug is being absorbed, the
greater the concentration gradient and faster the absorption rate.
• Altered Drug Distribution: Some drugs are
highly bound to plasma proteins, for example, coumarins, sulphonyl ureas, and
phenytoin. Co-administration of a drug,
which can displace the former from their binding sites, will cause an
increased pharmacological activity and possible toxicity. Trichloroacetic acid,
a metabolite of chloral hydrate, may displace warfarin from its binding sites
(plasma proteins) and so increases the anticoagulant activity which results in
bleeding tendency. Similarly,
methotrexate, an anticancer drug, is displaced by some sulphonamides and a
granulocytosis may result.
Altered Drug Metabolism:
• Induction of Hepatic Microsomal Enzymes:
Certain drugs, e.g. barbiturates,
alcohol, phenylbutazone, and some anticonvulsants are potent inducers of
hepatic microsomal enzymes. The simultaneous use of these drugs with any other
drug, which is normally metabolized by
this route, will result in increased metabolism or clearance of the latter with
reduced therapeutic efficacy if the parent compound is the effect mediator but
possibly increased if the effect is due to a metabolite. For example, the interaction
of barbiturates with warfarin results in decreased anticoagulant effect.
Interaction of tolbutamide with alcohol/ phenytoin/ rifampicillin results in decreased
hypoglycemic effect.
• Inhibition of Hepatic Microsomal Enzymes:
Some drugs inhibit the activity of microsomal enzymes and so the metabolism of
other drugs. For example, allopurinol, a
potent inhibitor of xanthine oxidase, reduces the metabolic or clearance rate
of 6- mercaptopurine which may cause
bone marrow depression if the dose of the latter is not reduced.
Altered Drug Excretion:
• Competition for Active Tubular Secretion:
Active tubular secretion of many drugs occurs in the proximal limb of the loop
of Henle. If two drugs, which are normally secreted in this way, are
co-administered in large doses, competition may lead to an interaction whereby
greater-than-expected amounts of one or the other are retained in the body. For
example, interaction occurs between probenecid and penicillin in which
probenecid is used to prolong the action of penicillin.
• Change in Urine pH: Reabsorption of the drug
is decreased in the renal tubule by changing the pH of urine. It is most likely
encouraged, for example, in salicylate or phenobarbitone poisoning where
alkalization of the urine will increase elimination of these drugs, are used to
increase elimination of these drugs. Similarly, pressure acidifiers, e.g.
ascorbic acid and ammonium chloride, are used to increase the elimination rate
of amphetamine, fenfluramine, and quinidine.
Pharmacodynamic Drug Interaction
• Drugs Having Similar Pharmacological Effect:
A patient receiving hypnotics may develop an allergic skin reaction and for
this, he receives an antihistamine which itself has a central nervous system
depressing effect. The combined effects may be sufficient to produce serious
sedation which cannot be obtained from either of these drugs. A similar effect is observed with the use of
hypnotics and alcohol (increased CNS
depression), narcotic analgesics and tranquilizers (increased CNS
depression), digoxin and quinidine (bradycardia), β-receptor stimulants, and
theophylline.
• Drugs Having Opposite Pharmacological Effect:
When a patient is receiving pilocarpine (cholinergic drug) for glaucoma (eye
disease) and at the same time for abdominal pain may be prescribed with an
anticholinergic drug, then interocular pressure may be altered by the
anticholinergic drug.
• Change in Electrolytic and Fluid Balance:
Drugs, e.g. diuretics, that cause potassium depletion may potentiate the effect
of digitalis and non-polarizing muscle relaxant but antagonize the effect of
lignocaine, quinidine, and procainamide.
