Communication is the transfer of information meaningfully to those involved. It is the process in which, messages are generated and sent by one person and received and translated by another person. The communication process between health professionals and patients serves two primary functions:
1. It establishes an ongoing relationship between the
professional and the patient.
2. It provides the exchange of information necessary
to assess a patient’s health condition, implement treatment of medical
problems, and evaluate the effects of treatment on a patient’s quality of life.
Rules for Designing a Good Counseling Session:
Some important things should be kept in mind to design
a successful counseling session. These are:
1. Developing a professional image by dressing
formally and sitting properly, i.e. neither leaning nor sitting erect.
2. Having eye contact with the patient, but also at the same time avoiding starving.
3. Establishing rapport with the patient by
introducing himself and shaking his hand.
4. Starting the counseling session with the
pre-determined plan which must include questions to identify the patient’s
problems.
5. Attempting to keep the session on tract while
answering the queries raised by the patients.
6. The counseling session should include a greater
number of open-ended questions as compared to close-ended questions.
7. The counselor should have clarity of speech and
patience.
8. The session should be ended gradually and not
abruptly and ample time should be given to the patient to express and clear his
doubts.
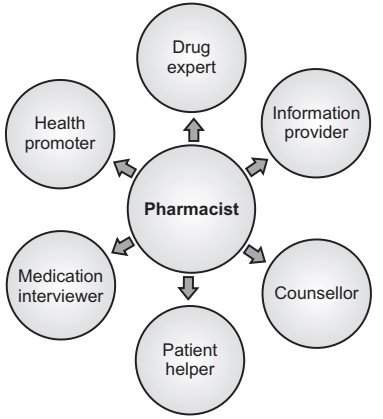 |
| Fig.1: Role of Pharmacist in Patient Counseling |
The following are the steps to be followed during
patient counseling:
1. Preparing for the session
2. Opening of the session
3. Counseling content
4. Closing the session
Process Steps (Preparing for the Session and Opening of the Session)
1. Established caring relationships with patients as appropriate to the practice setting and stage in the patient’s health care management.
• Introduce yourself as a pharmacist.
• Explain the purpose and expected length of the
sessions.
• Obtain the patient's agreement to participate.
• Determine the patient’s primary spoken language.
2. Assess the patient’s knowledge about his or her
health problems and medications, physical and mental capability to use the
medications appropriately, and attitude towards the health problems and
medications.
• Ask open-ended questions about the purpose of each
medication and what the patient expects and ask the patient to describe or show
how he or she will use the medication. They should also be asked to describe
any questions, concerns, or uncertainties they are experiencing with their
medications.
3. Provide information orally and use visual aids or
demonstrations to fill the patient’s gaps in knowledge and understanding.
• Open the medication containers to show patients the
colors, sizes, shapes, and marking on oral solids.
• For oral liquids and injectables, show patients the
dosage marks on the measuring device. Demonstrate the assembly and use of
administration devices such as; nasal and oral inhalers.
• As a supplement to face-to-face oral communication,
provide written handouts to help the patient recall the information.
4. If a patient is experiencing problems with his or
her medications, gather appropriate data and assess the problems. Then adjust
the pharmacotherapeutics regimens according to protocols or notify the
prescribers.
5. Verify patient’s knowledge and understanding of
medication use. Ask patients to describe or show how they will use their
medications and identify their effects.
Observe patient’s medication use capability and accuracy and attitudes
toward following their pharmacotherapeutics regimens and monitoring plans.
Counseling Content
1. The medications trade name, generic name, common synonym, or other descriptive names and when appropriate, their therapeutic class and efficacy.
2. The medications use and expected benefits and activities.
This may include whether the medication is intended to cure a disease,
eliminate or reduce symptoms, arrest or slow the disease process, or prevent
the disease or a symptom.
3. The medication's expected onset of action and what to do if the action does not occur.
4. The medications route, dosage form, dosage, and
administration schedule (including duration of therapy).
5. Directions for preparing and using or administering
the medication. This may include; adaptation to fit patient’s lifestyles or
work environments.
6. Action to be taken in case of a missed dose.
7. Precautions to be observed during the use or
administration of the medication and the medication's potential risks about
benefits. For injectable medications and administration devices, concerns about
latex allergy may be discussed.
8. Potential common and severe adverse effects that
may occur, actions to prevent or minimize their occurrence, and actions to take
if they occur, including notifying the prescriber, pharmacist, or other health
care provider.
9. Techniques for self-monitoring of pharmacotherapy.
10. Potential drug-drug (including non-prescription),
drug-food, and drug-disease interactions or contraindications.
11. The medication's relationship to radiologic and
laboratory procedures (e.g., the timing of doses and potential interferences
with the interpretation of results).
12. Prescription refill authorizations and the process
for obtaining refills.
13. Instructions for 24-hour access to a
pharmacist.
14. Proper storage of the medication.
15. Proper disposal of contaminated or discontinued
medications and used administration devices.
16. Any other information unique to an individual
patient or medication.
Patient Counseling Aids
A pharmacist can use different aids to bring about
effectiveness in counseling patients.
These aids can be exemplified by the use of medication cards, pictograms,
and patient information leaflets.
